The future of healthcare starts with precise data analytics. Healthcare organizations are revamping their investments in precision medicine and big data analytics to improve patient outcomes. Despite recent advancements to implement these data models into clinical systems, there are still obstacles to their adoption on a global scale.
Nowadays, technological advancements allow for merging and collecting large datasets from multiple sources, including electronic health and medical records (EHR/EMR), wearable health devices, personal health records (PHR), and so much more. Complex algorithms, supported by high-performance computing power, enable these large datasets to be transformed into knowledge that can be leveraged in precision medicine models.
Precision medicine encompasses both technical and sociopolitical aspects about disease treatment and prevention. This means that for health scientists and researchers to draw scientific conclusions on disease treatments, preventative care methodologies, and create new medications, they need accurate data.
The biggest challenge that the healthcare industry faces is how to improve the organization and implementation of these large datasets so that health science can continue to progress.
Major Health Data Access Barriers
Medical records include in-depth personal data related to one’s physical and mental health status, both past and present. This data is heavily guarded and not available to the public.
Medical record data is usually siloed in hospital or clinical charts without any central sharing to allow the volume of data required to exploit big data science methodologies.
The current technical infrastructure for moving, manipulating, and managing medical data is not readily available, so significant barriers exist when trying to access this type of data.
Several areas need to be addressed in order to improve the translation of existing medical data into new tech-powered healthcare solutions. A few of these areas include:
- Curation of clean medical data
- Collections & standardizations of heterogeneous datasets
- Informed consent for the use of de-identified health data & information
- The ability for healthcare and research communities to leverage/access to this data for further use.
Integrating large datasets across multiple sources and domains is a daunting task. The heterogeneity in the data syntax, numerous data structures of schemas, and ambiguous semantics cause many issues for this type of data integration.
How Do We Fix These Issues?
How can we harness the power of big data and AI to improve healthcare for all?
Large volumes of medical information could be repurposed to identify novel risks or therapeutic treatment options applicable at the individual level to improve health-related outcomes.
Let’s take a look at some practices revolutionizing the core concepts of healthcare.
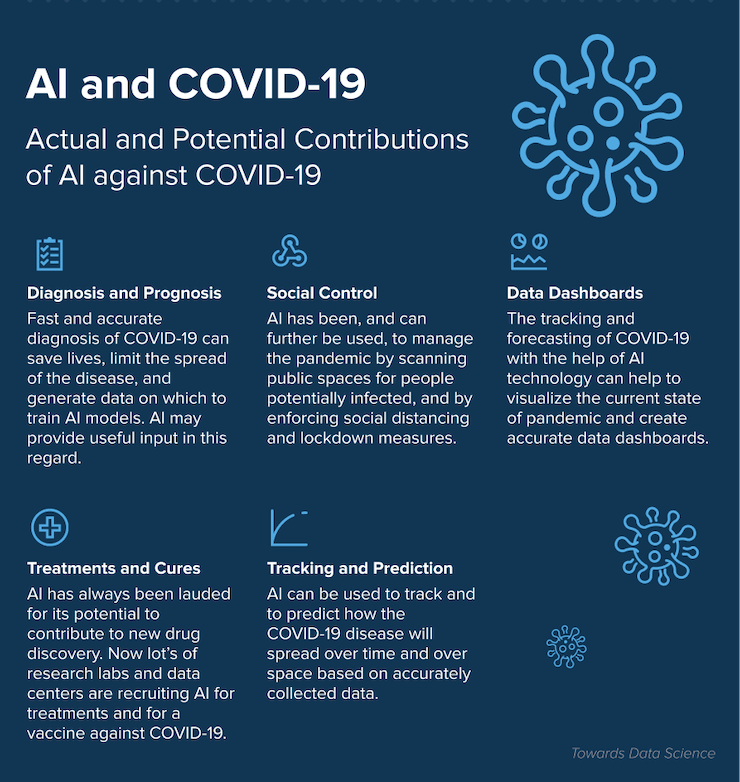
It’s safe to say that the COVID-19 has changed the healthcare sector in many ways. It has speeded up the digitization of the industry. AI has proven efficient to combat the spread of the deadly virus around the world and make the working environments safer and healthier for frontline workers. Take a look what AI has to offer during the pandemic times:
Data Capture Impacting Precision Medicine & Precision Public Health
To be as accurate and precise as possible, medicine must revolve around information gathered from a myriad of sources. This means going beyond genetic data and exploring more nontraditional data.
Individualized treatment is not the sole component of precision medicine. Precision medicine refers to disease prevention, differential diagnosis, and disease treatment through immutable (genetics) and actionable (behavior) factors.
Several types of biological and environmental factors come into play when gathering data for precision medicine. Here are some of the main factors involved in precision medicine.
- Electronic Health Records (EHR) – the most widespread application of big data in medicine, involving a digital record of every patient’s medical history, laboratory test results, demographics, allergies, and medications.
- Personal Health Records (PHR) – a collation of all health information provided by different healthcare providers, directly accessible by the patient in a cloud-hosted environment.
- Social Networking Platforms – combines behavioral and social domains of data-rich environments considered in the context of precision public health (dietary habits, psychological attributes, lifestyle choices, sleep patterns, etc.)
- Patient-Generated Data – physical activity, dietary intake, blood pressure levels, blood glucose levels, lifestyle choices, and other similar variables collected using wearable health devices and smartphones. All this can be collected and analyzed with predictive analytics solutions.
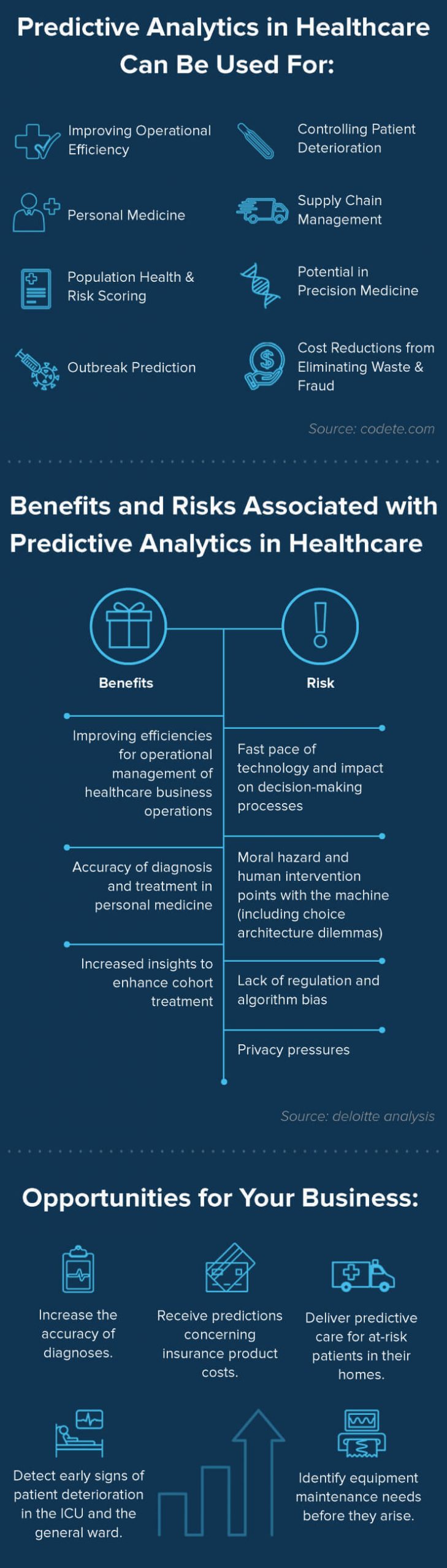
Predictive analytics comes in handy, when there’s a need to analyze large volumes of data and make predictions. A good example in this area can be period tracker apps. With the consent of the user, these apps collect and process period and fertility data, then make assumptions on the next period day. And that’s just a start! The user also gets practical insights on physical and mental health, tips on conceiving and pregnancy, and more.
Based on the information the user provides (past period days, medication, body temperature, mood, sexual activity, birth control), predictive analytics analyzes it and predicts the next menstrual cycle or hints at possible diseases. The technology empowers period tracker apps helping women around the world address health and wellness.
Take Flo, a well-known app in the Femtech industry. Flo is a data-driven mobile app for period tracking and daily health insight generation. The Flo’s period prediction accuracy lies in artificial intelligence and predictive analytics. These two technologies analyze data they get and make predictions. The value women get is immense. Using the app, they not only get AI-driven period and ovulation prediction, but get more educated about their physical and mental health.
To know more about other benefits of predictive analytics and its use in healthcare, take a look at our infographic:
AI & ML for Big Data Analytics in Precision Medicine
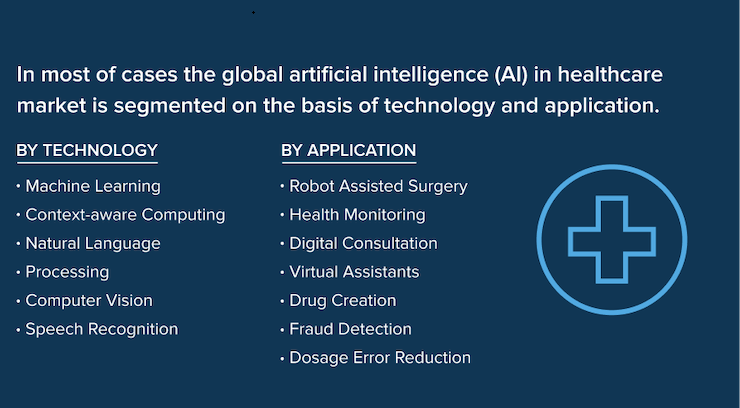
Healthcare institutions are well equipped with different sets of information technology such as Artificial Intelligence and Machine Learning. There is much information leveraged by the healthcare industry, from electronic and personal health records (EHR/PHR) to laboratory and health information systems (LIS/HIS).
AI-driven solutions are the answer when it comes to data collection and analysis in the clinical settings. This can then undergo multiple pre-processing techniques to apply big data techniques, including machine learning and artificial intelligence (AI). As a result, these technologies not only help store and analyze medical information but detect anomalous actions.
Anomaly detection helps recognize abnormal physiological readings, and the patient’s response to treatment. It also improves patient care and decreases the healthcare worker load.
Big Data Genomics and Precision Medicine for Cancer Research
Big data genomics and precision medicine go hand-in-hand, especially when referring to cancer research.
Cancer researchers have a lot of high volume, high variability, and high-velocity data to leverage. Big data analytics are a researcher’s primary ally, from genetic information and physiological sensor data (wearable health monitoring devices) to structured and unstructured clinical data.
The increasing availability of clinical data and emerging molecular profiling technologies have accelerated cancer precision medicine throughout the nation.

Source: Unsplash
According to the study published in the Journal of Clinical Oncology Clinical Cancer Informatics, a big data analytics tool that mines large datasets of various types of cancer or cancer-related diseases could help researchers identify patterns in potential treatment options and significantly accelerate precision medicine.
Developed by researchers at the University of Michigan Rogel Cancer Center, this big data analytics tool combines multiple datasets to transform medical information into meaningful clinical insights.
Structured data used for statistical analysis has created the gold standard for cancer research and testing efficacy. Cancer researchers rely on “clean data” to produce the results they need to discover cures and various treatment options.
Unstructured clinical data is cheaper to collect than structured data. It’s useful for assessing the results of interventions on several different levels, rapid searches, inexpensive storage, and valuable hypothesis generation without having to be “clean.” There are limitations to both structured and unstructured data, however. Structured data is typically costly to produce, while unstructured data is much cheaper, but is often incomplete, ambiguous, doesn’t always capture essential variables, and must undergo structured conversions to be utilized in predictive modeling and statistical analysis.
Despite the limitations to clinical data aggregation, big data is massively informative in precision medicine. Precision medicine continues to supercharge the role of big data analytics in cancer research, given the strong influence of patient-level genomics.
Many healthcare institutions are paving the way for precision medicine using big data analytics techniques to develop patient population-based, cause-and-effect models from genomic data.
Bottom Line
According to the market research, the precision medicine software market is expected to grow from $1.2 billion to approximately $2 billion by 2024. The big data market is expected to reach over $123 billion by 2025! These numbers speak for themselves – big data is a major player in the game of medicine.
Many healthcare organizations are already integrating advanced precision medicine tools and machine learning apps into their clinical practices.
Investing in new technologies or implementing new practices is always a risk. However, if the technology supports a healthcare organization’s specific needs concerning improving healthcare and precision medicine, then the costs are well worth the risk.
Hopefully, clinical professionals and software engineers can discover new innovative ways that make it easier to aggregate clean data for big data precision medicine in the near future. In the meantime, big data in medicine has significantly impacted healthcare organizations from a business standpoint.